Varicose veins are dilated veins under the skin of the leg. These abnormal veins are common, not dangerous, but may cause a number of symptoms.
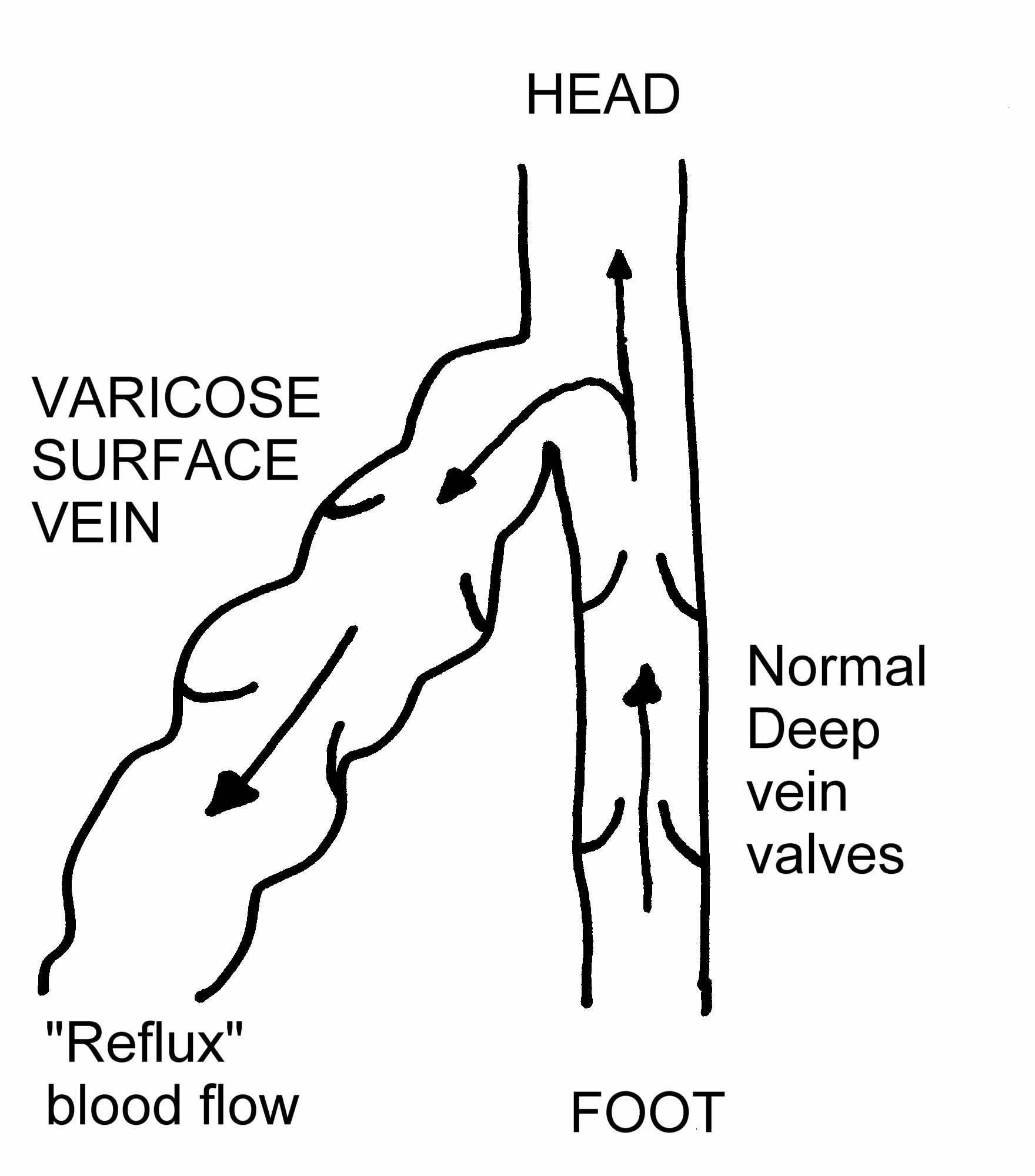
Normal veins rely on valves to keep the blood moving upwards. In varicose veins these valves do not function and the flow of blood is slow or even reversed. In order to treat varicose veins successfully the faulty valves need to be dealt with in addition to removing or reducing the varicosities. Two important sites where faulty valves occur are the groin or behind the knee. The function of the veins is assessed by an ultrasound scan (Duplex).
What problems do Varicose veins cause ?
The pressure in the veins especially when standing can lead to pain, swelling, and may sometimes lead to skin changes (brown staining, eczema, ulceration). Varicose veins sometimes develop a clot (thrombosis) causing the vein to become red, hard and tender, known as “phlebitis”. If injured varicose veins are prone to cause bruising or may occasionally bleed.
What causes Varicose Veins ?
There are several possible factors:
- Inherited vein wall weakness
- Faulty valves
- Prolonged standing (occupational)
- Raised venous pressure and hormonal effects in pregnancy
- More common as we get older
- After damage to the deep veins of the leg (ie DVT)



What are the possible Treatments ?
Many patients improve with simple measures,
- EXERCISE. Walking, running, cycling and swimming are all beneficial. Walking is the simplest to do and using the calf muscles directly pushes blood up the veins of the leg improving the circulation.
- AVOID standing still for long periods of time.
- ELEVATE the legs whenever possible. Any elevation will help but if you can raise the feet above the level of the heart (chest) this will be particularly beneficial.
- If you are OVERWEIGHT, try to reduce this down towards your ideal/target weight.
- Use firm "graduated" SUPPORT STOCKINGS on the legs during the day. These can be brought at chemists or obtained on prescription. The pressure in the stocking is designed to be greatest at the ankle level and gradually decrease up the leg. This assists the return of blood up the veins. A below knee stocking is often sufficient.
FOAM SCLEROTHERAPY
 Some chemical agents when injected into veins cause them to become inflamed, and with time, scarring occurs leading to obliteration of the vein. Veins with faulty valves and varicisoites can be treated in this way. This is called sclerotherapy and has been practised for many years. Mixing the chemicals with air to make a foam is a more recent development which gives better results. Modern ultrasound can be used to direct the foam into the correct vein also improving results. Foam sclerotherapy can be performed in a clinic and does not require any anaesthesia. Following the treatment it is important to wear a bandage and/or a support stocking on the leg for 2 weeks. Success rates are approximately 70 – 80%. If the veins do not disappear the treatment can be repeated. Side effects can be due to reactions to the foam entering the general circulation. With care these reactions are uncommon and transient. Local “phlebitis” of the treated vein (inflamed thrombosis) can cause pain for 1-2 weeks and may occasionally leave some marking on the leg.(10-15%).
Some chemical agents when injected into veins cause them to become inflamed, and with time, scarring occurs leading to obliteration of the vein. Veins with faulty valves and varicisoites can be treated in this way. This is called sclerotherapy and has been practised for many years. Mixing the chemicals with air to make a foam is a more recent development which gives better results. Modern ultrasound can be used to direct the foam into the correct vein also improving results. Foam sclerotherapy can be performed in a clinic and does not require any anaesthesia. Following the treatment it is important to wear a bandage and/or a support stocking on the leg for 2 weeks. Success rates are approximately 70 – 80%. If the veins do not disappear the treatment can be repeated. Side effects can be due to reactions to the foam entering the general circulation. With care these reactions are uncommon and transient. Local “phlebitis” of the treated vein (inflamed thrombosis) can cause pain for 1-2 weeks and may occasionally leave some marking on the leg.(10-15%).
Mechanico-chemical vein ablation is where the sclerosant chemical is delivered directly into the faulty saphenous vein trunk with a catheter that also physically spins and sliightly damages the lining of the vein. This combination is desgined to increase the success rate for obliterating the vein. The potential advantage of this is that it is less uncomfortable and needs less local anaesthetic than the thermal techniques (see next section). The long term durability is still being evaluated for this technique.
Endothermal Ablation
EndoVenous Laser Ablation (EVLA) and Readiofrequency Ablation (RFA) are techniques for treating varicose veins. These procedures seal off the main underlying faulty vein that is feeding the varicosities. This will be either the Long saphenous Vein (LSV) in the thigh or the Short Saphenous Vein (SSV) behind the knee and calf. The traditional operation was to tie and strip these veins. These ablation techniques have replaced that surgery and are less painful with quicker recovery.
EVLA and RFA are techniques to remove the LSV and SSV from the circulation without a wound and without stripping. Both these treatments can be performed under local anaesthesia. A catheter is passed up the vein from the ankle or knee level. It is carefully placed at the junction between the LSV/SSV and the deeper veins. An ultrasound scan is used to place the catheter precisely. When the catheter is activated in contact with the vein wall either an electrical current or laser energy is passed through the vein wall. This causes the proteins in the vein wall to change shape and contract down. The catheter is slowly pulled back down the vein. This leaves the vein contracted down and no blood flows through it. It is effectively removed from the circulation achieving the same outcome that stripping of the vein does in traditional surgery. Long term follow up has shown that the veins largely remain closed off and rarely open up again.
Further new ways of occluding the LSV and SSV are being introduced. A form of glue gan be used to seal the vein off. This requires no anaesthetic which may be a benefit. THe long term durability of this treatment is under evaluation.
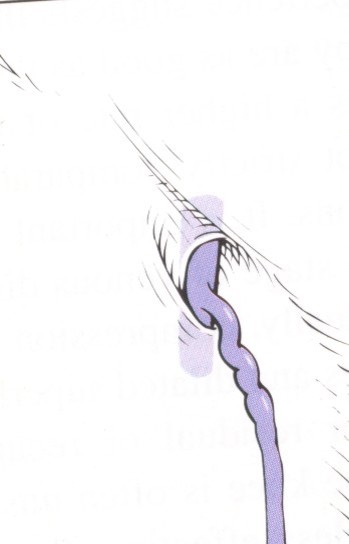
Phlebectomy or Avulsion of veins.
The actual lumpy surface varicosities can be removed, pulled out, by small surgical procedures. This is usually done through a series of small cuts (2-4mm). The terms "avulsions" or “phlebectomy” are used to describe this. The veins are removed in sections (avulsed) through each of the incisions.
After Care
Most procedures are now day case or clinic treatments. Staying overnight is rare. The leg(s) will be firmly bandaged to reduce bruising and help healing. After 1-2 days the bandage may be changed for a stocking which is worn for 5-7 days. For the first few days it may be easier to wear the stocking day and night. After this if the leg is comfortable without it at night, you can use the stocking just during the day. Aim to either rest with the leg elevated moving the ankle, or be up on the move around the house and garden. Avoid standing for any long period of time; avoid crossing your legs. A daily walk of 1-2 miles should be possible.
After the ablation procedures the treated deeper vein may become sore after 3-5 days. This is part of the reaction to the treatment and will settle. Anti-inflammatory pain killers will help with the discomfort for a few days. After phlebectomy the small cuts on the leg will usually be closed with skin glue or tape rather than stitches. Where stitches are used they are usually dissolvable.
Complications
Recovery from RFA or EVLA alone without any phlebectomies can be quite quick in 2-4 days. Phlebectomies in addition will inevitably produce some bruising and soreness. The severity depends on how many veins are removed. Most of the soreness will settle in 3-5 days. Full clearance of the bruising will take longer. Small nerves next to the veins can be disturbed leading to patches of numbness in the lower leg and foot in approximately 10% of patients. This slowly resolves but is occasionally permanent. A thrombosis can occur in the deeper veins of the leg (DVT) but this is not common, affecting less than 1% of patients. Keeping mobile after the procedure and wearing the stocking help reduce the risk of this. Infections in the very small wounds are uncommon.
For more information click HERE