Vascular Unit Updates
Bristol Bath Weston Vascular Network
Marcus Brooks, Consultant Vascular Surgeon, North Bristol NHS Trust
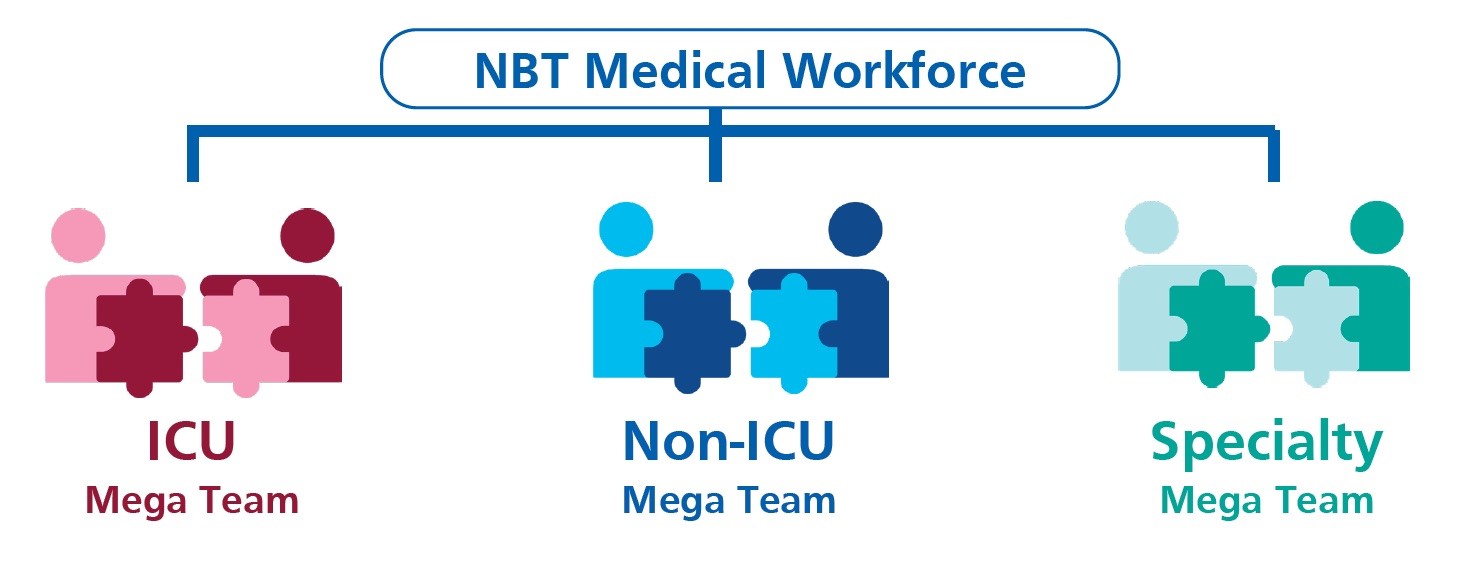
From last Tuesday vascular consultants were redeployed into a ‘Speciality Mega Team’ with two consultants each week allocated to the ‘Non-ICU Mega Team (NIMT)’. All but one vascular junior doctor has been re-deployed to a Mega Team. The specialist vascular ward has closed. Vascular outpatient clinics have been cancelled or are conducted over the telephone. Vascular inpatients now looked after by a NIMT consultant with input from a vascular surgeon. Urgent vascular cases are seen on the surgical admissions unit or in a Monday to Friday ‘hot clinic’. The diabetic foot service continues to deliver face-to-face reviews with specialist nursing, podiatry and vascular specialist input.
We recognised how essential teamwork, communication and staff well-being are in a constantly changing situation. We have Mon-Fri meeting using Microsoft Teams which is accessed remotely if not needed in the hospital. These meetings are joint with interventional radiology, podiatry and specialist vascular nurses. These meetings replace the weekly network face to face MDT. Discussions are documented using ‘refer-a-patient’, which was introduced into the Trust in response to COVID-19. Refer-a-patient also allows us to document the management of all of our acute referrals and urgent operative planning.
The South West has not seen the surge of COVID-19 cases experienced in some regions. Southmead Hospital Bristol at the end of last week had 90 COVID positive patients at with 15 patients intubated. Gloucester and Exeter are the regions hospitals most affected by COVID-19. In other SW units, operating is on emergency cases only, the junior team has been reallocated and inpatients have been moved into shared surgical wards. Most units have had consultants self-isolating, the majority now returned to work.
We are perhaps starting to see an impact of delayed hospital presentations. Our patients don’t want to come into hospital. In Bristol, whilst the ‘hot clinic’ is busy, however, referrals from the stroke team are significantly reduced. Other SW similarly report a reduction in vascular admissions, most carotid work has ceased, and CLTI patients are presenting late.
Special mention must go to Andy Weale, Rebecca Winterborn and Rob Hinchliffe for the enormous effort they have put in to ensure the continuity of the specialist vascular service, reorganisation of wider surgical services and creation of a package of well-being support. The importance of mental health was driven home last week when a junior doctor at a network hospital took their own life. We are all working outside our normal practice and share concerns regarding the safety and health of ourselves, family, friends and colleagues.
The huge positive for me has been seeing the vascular team responded to this challenge. Despite re-deployment to other wards our fabulous nursing team remain upbeat and look forward to when they can return to specialist vascular nursing. The flexibility of colleagues and willing ness to take on new commitments has been inspiring. At a Trust level whilst plans have been slow to evolve at times there is a real sense of purpose, combined with care for patients, their families and staff. Both ICU and Medicine have run staff education packages and we have PPE stations across all patient areas.
There has been improved joined up working across SW healthcare organisations. This is most evident in the creating of the NBT led Nightingale Hospital at the University of West of England, which is staffed from across the South West.
This pandemic may yet impact on our waistlines. The Trust provided an Easter egg for all staff, Krispy Crème have delivered donuts and the ‘Jolly Hog’ provide sausage sandwiches and pork rolls at weekends. Many staff are baking and bringing in cakes. We have at least had lovely weather for getting out on the bike or running on the Downs!
Our thoughts in the South West are with colleagues working in regions more severely affected by the pandemic. We are enormously grateful for the advice and learning that they have shared. It looks at the moment that in the SW social distancing has been effective. This is perhaps due to its timing, the rurality of many of our communities and limited public transport networks. Our challenge may therefore be more how we manage patients who are presenting later and how best deliver our specialist vascular services during a prolonged recovery period during which further COVID-19 spikes occur.
12th May 2020
A view from Cambridge – Jon Boyle, Consultant Surgeon
Cambridge Unit Report
Cambridge benefitted from its relative geographic isolation, low population density and the instigation of National Lockdown before Covid-19 became widely prevalent in the East of England.
Elective operating and outpatient clinics ceased on 20th March. Addenbrookes peaked at approximately 150 inpatients with Covid-19 of which just fewer than 50 were treated on intensive care. In the last two weeks the number of inpatients has fallen to approximately 100 with 25 on intensive care. The hospital has been running with approximately 400 empty beds for most of this period, although this number has dropped over the last couple of weeks.
Vascular Outpatients
All regular clinics have been converted to telephone consultations. Urgent vascular problems have been dealt with by a combination of telephone call to patients, GPs and other specialists, the facility to send images through the specialist nurse team and the CLI clinic. Prior to Covid-19 the CLI clinic ran twice a week for 4 patients per clinic led by the specialist nurses and supported by a vascular technologist and vascular surgeons. This clinic now runs every day, with a maximum of 6 patients seen face to face with duplex imaging as required, mainly for CLI cases, but also large AAAs and symptomatic carotids. It has got significantly busier in recent weeks.
Vascular Surgery and Angioplasty
There was an initial significant reduction in theatre capacity at Addenbrookes from 48 daytime operating theatres to 6. This led to a reduction in vascular theatre capacity to between 8% and 15% of the normal weekly envelope. From this week, however we are back up to 50% capacity and have access again to overnight recovery HDU beds, which will allow carotid and open aortic surgery to restart. One of the two angiography suites is closed and the loss of radiographers to the ED Covid rotas has and will continue to limit endovascular procedures in the hybrid theatre. Cambridge University Hospitals has followed RCS and VS Guidance around PPE and all operations are performed with the entire team wearing FFP3 masks and associated protection.
Staffing
One of the biggest challenges has been around staffing. The loss of all junior staff, who have been assimilated into ward teams has resulted in a consultant delivered service. We have developed two teams of 4 consultants who cover vascular emergencies and the CLI clinic 24/7 on alternate weeks. This can be particularly onerous for the first on call consultant out of hours. We run a daily 45-minute handover Zoom meeting for the day and night teams to discuss inpatients and urgent outpatient problems. There has been a significant impact on training, however two NTN trainees have been supporting the CLI clinics and emergency operating lists.
Non-arterial Centres and Papworth
Referrals from Papworth have increased, particularly for Covid-19 patients on Ecmo, with thrombotic problems and bleeding. All non-arterial centre outpatient work is being undertaken remotely, with urgent cases being seen at the Addenbrooke’s CLI clinic. Angioplasty for CLI cases is still being undertaken on a case-by-case basis in two spoke hospitals. All varicose vein interventions have ceased.
Overall the vascular team members, surgeons, specialist nurses and vascular technologists have worked closely together to maintain a service for patients with urgent limb or life threatening vascular problems. The challenge now will be to maintain team working as the service expands and returns towards pre-Covid practice.
27th April 2020
A view from York - Paddy McCleary, Consultant Surgeon
We have a unit covering 800 000 across North Yorkshire on a hub and spoke model. The hub is in York with the two main spokes in Scarborough (50 miles away) and Harrogate (25 miles away). At the moment we have 6 consultants and 5 middle grades.
I suspect we were running 2-3 weeks behind London in the pandemic timescale and therefore because of the relatively early lock down, we have not had the tsunami of cases in North Yorkshire. We have had approximately 80 hospital deaths which seem to have plateaued. ITU is not full and there are empty beds in the hospital.
All elective surgery and outpatient appointments were stopped 4 weeks ago. The local Treatment Centre was closed completely and the local Nuffield was closed to private practice but prepared for NHS work. Non Covid ICU was moved to PACU. Theatre nurses and ODP’s were trained to work on ICU. Consultant anaesthetists also received ICU refresher training.
We run 4 theatre lists per day: Emergency list, Surgical CEPOD, Vascular CEPOD and Trauma.
There are theatre meetings every morning at 8.30 am and 3.30 pm chaired by the lead Covid surgeon of the day. The Covid surgeon is one of the more senior surgeons who will not have any other commitments that day. He effectively referees. At the 3.30pm meeting a decision is made as to whether there will be space on one of the lists to perform a cancer case the next day.
In vascular we have split into 3 teams of 2 consultants with 2 middle grade surgeons. The teams do not meet to reduce the chances of everyone becoming unwell at the same time. 3 of us have had Covid (but not tested). We work on a 3 weekly rota. Handover by Zoom on Monday am.
Team 1: Based on the ward for emergencies. Emergency OPD in York everyday with one clinic/ward visit in Scarborough and Harrogate per week.
Team 2: Office based. Checks all correspondence, referrals and results. Conducts telephone follow up.
Team 3: Rest week
We have set up a Virtual Ward to manage emergencies as outpatients with urgent imaging and endovascular intervention as required.
We are still performing carotid surgery according to our usual practice of local anaesthetic, no critical care, 24hr stay. However, we are being more selective. We are performing bypass for critical ischaemia, foot debridement and amputation at a slightly reduced rate compared to normal but the service for critical ischaemia is better than normal due to emergency clinics every day and improved radiology capacity.
We have repaired one 8cm with EVAR who was readmitted 1 week later and died of Covid.
Our Trust is following PHE Guidelines for PPE (7th April). Therefore, we are only using PPE 2 for surgeons and nurses in theatre. Anaesthetists use PPE 3 for intubation and extubation.
We have not been required to assist on ICU as yet and it is more likely that we will be required to assist on Covid wards if the situation escalates
Overall our Trust responded early to the threat of Covid with a very well-coordinated plan led by some very capable clinical colleagues. Testing for Covid has been almost impossible to access for staff, we are short of theatre scrubs and PPE is being rationed.
13th April 2020
A view from the Black Country - Andrew Garnham
With accelerating levels of covid in the Midlands those of us working here have a level of trepidation looking at London. We have stopped our routine work and share an emergency and urgent theatre with other specialties. Although there has been some confusion around the use of PPE we are seeing adequate supplies, although conversations with our senior managers outline the strain on the supply chain.
We have changed our practice going to largely virtual clinics and seeing a small number of patients in person and having a rota that assumes some of us will be ill or self-isolating. I am sure we are all having those anxiety provoking conversations around critical limbs where the patients are sitting at home not wanting to come in or having a conversation around the additional risk of attending the hospital. On a personal note I will share the anxiety of having what I think was the virus although before widespread testing, so there is that doubt around have I actually had it?
I spent a strange week last week on my return covering a colleague who was forced to self-isolate his wife also a clinician having been ill. I found the performance of surgery even an amputation in full PPE an uncomfortable challenge and the delivery of said colleague’s provisions a welcome distraction.
We are now starting to think that we are seeing the effects of self-isolation with numbers of patients coming in at a high steady but manageable level. Now we are even talking in our local consultant meeting on zoom around how we might restart urgent elective surgery as the covid crisis stabilises. Changes look to be upon us for a while to come.
I hope you all remain well out there and I like your other members are happy to talk.
7th April 2020
St Mary's Hospital - Michael Jenkins
As of Monday 6/4/20, we have 352 Covid 19 positive patients at Imperial with 96 level 3 ventilated patients. ITU is already well beyond its normal bed base in the current Surge 1 phase of up to 143 ventilated beds. Over the next two weeks there are plans to expand by another 157 ventilated beds. Other areas including PICU, theatres, recovery and the endoscopy unit will be brought on stream as needed. A&E has been divided into a Red (known or suspected Covid +ve) and a Green zone for other cases and as an MTC we remain open to trauma from within the region. Our anaesthetists continue to cover 4 emergency theatres and man a “Covid intubation team” with resident Consultants round the clock. On a more positive note, 406 Corona virus patients have recovered and been discharged over the last few weeks.
From a vascular perspective, we are running an emergency service with our current on call and Consultant of the week systems in place. SPRs remain attached to vascular, but other juniors have been re-deployed to a wider pool. We have now got authority to perform urgent NHS vascular surgery at the Bupa Cromwell hospital with Crown indemnity and will encourage our SPRs to attend to maintain training. Individual outpatient clinics are telephone only with the provision of having one or two “hot clinics” per week for patients who need to attend in person for all to use as needed. Some surgeons (mostly vascular in fact) have volunteered to help the ITU effort and are currently going through training and induction with a plan to commence taking responsibility for ITU shifts (4 day week and 3 day weekend the following week) later this week pending need.
On a lighter note, there are some advantages to the current situation – only essential meetings continue; there is a feeling of camaraderie in the hospital; local restaurants are donating and delivering food and there is much less traffic!